Understanding the genetic causes of prostate cancer
June 2022
We are enormously grateful for the generosity of Cancer Research and Genetics UK over the years in supporting The Institute of Cancer Research’s (ICR) prostate cancer research. We hope you will now continue your support with a further donation towards the cutting-edge prostate cancer research led by Professor Ros Eeles.
Your support is critical as more than 52,000 people are diagnosed with prostate cancer every year in the UK, and around 22,000 patients are considered at “high -risk” of their cancer spreading. The number of men diagnosed with the disease has also been increasing over the last ten years as more men get tested and the population continues to age. 12,000 men will lose their life to prostate cancer each year in the UK leaving their loved ones devastated.
UK Genetic Prostate Cancer Study
The UK Genetic Prostate Cancer Study (UKGPCS) was first established in 1993 and is the largest prostate cancer study of its kind in the UK, involving nearly 200 hospitals, including our clinical partner, The Royal Marsden NHS Foundation Trust. The study which is led by Professor Eeles of the ICR aims to find genetic changes which are associated with prostate cancer risk. If we can find alterations in genes that increase the chances of getting prostate cancer, it may be possible in the future to use this knowledge:
- To screen other family members to see if they are also at a higher risk of developing prostate cancer.
- To develop new prostate cancer treatments for the future.
The target is to recruit 26,000 men into the study by 2022 and so far, 22,947 men have been recruited.
Causes of prostate cancer
Although prostate cancer is the commonest cancer in men in the UK, with 1 in 8 men developing prostate cancer in their lifetime, its causes remain very poorly understood with few established risk factors.
The fact that prostate cancer incidence tends to be much higher in Western countries (for example the USA and UK), together with migrant studies, indicates that lifestyle and/or environmental factors such as diet could be important determinants of prostate cancer risk. However, so far little is known abou t which lifestyle factors might contribute to prostate cancer, and results between current studies are conflicting.
Part of the study involves collaboration with Professor Kenneth Muir at the University of Manchester who is conducting a study into which environmental factors might affect prostate cancer risk. Men taking part in the UKGPCS can also opt to take part in the environmental study if they wish by filling in a lifestyle questionnaire.
Genetic causes of prostate cancer
The UKGPCS was set up to find genetic alterations which occur in patients who have prostate cancer. A man’s risk of developing prostate cancer increases if he has a first-degree relative (father or brother) who was diagnosed with prostate cancer at a young age.
Therefore, the researchers are looking for men who are affected at a young age or who have a family history of prostate cancer, since it is more probable that these prostate cancers are due to an inherited genetic cause rather than an environmental cause.
All men who come to the Royal Marsden Hospital to be treated for prostate cancer are asked if they would like to take part in the study so that the researchers can also look to see if they find genetic alterations in older men, and those who do not have a f amily history of prostate cancer.
Ethical approval to continue to collect samples for the study is in place until the end of 2022 and this will be extended until 2027 once approved, as the study is being extended for another five years.
How you can help
The last decade has brought major advances in the way we diagnose and treat prostate cancer and men with advanced disease (those whose cancer has spread to other parts of the body) are living longer than ever. However, there remains an urgent need to continue our research to understand the causes of prostate cancer as more men are being diagnosed with the disease every year.
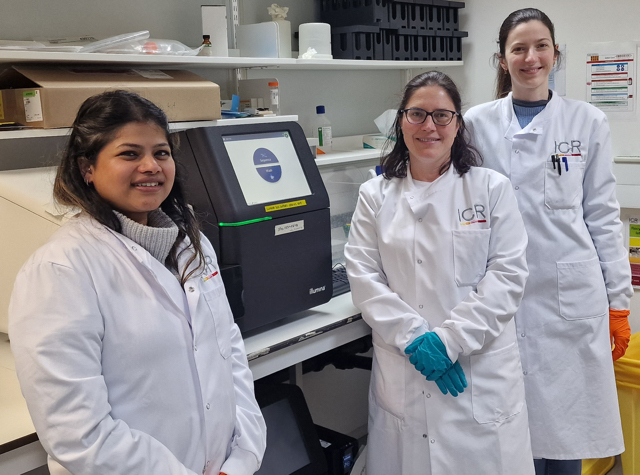
Professor Eeles and her team are striving to make further advances for the ultimate benefit of patients with prostate cancer all over the world. To do so, they need to secure funding for a new -80 freezer for their laboratory. This will allow them to safely store blood samples collected from patients enrolled onto the UKGPCS. Their current freezer is over 10 years old and needs replacing. If the freezer should break down the team would need to urgently decant the samples into a back-up freezer and then transfer them back into the original freezer once it has been repaired. This carries the risk of compromising the quality of the samples and thus negatively affecting the research. Following the latest engineer’s report, the team have been advised to purchase a new freezer as soon as possible as the current freezer is coming to the end of its lifespan.
We would be delighted if Cancer Research and Genetics UK would consider renewing their support of Professor Eeles’ vital research. A donation of £10,275 would allow the team to purchase a new freezer and safely store patient samples – the basis of the genetic research they undertake in this study.
Your kind support would enable Professor Eeles and her team to make further advances for the ultimate benefit of prostate cancer patients everywhere.


 The University of Liverpool has received another £10,000 donation from Cancer Charity, Cancer Research and Genetics UK (CRGUK), further securing the long-standing partnership which has seen the CRGUK donate over £70,000 to the University to help fund vital cancer research.
The University of Liverpool has received another £10,000 donation from Cancer Charity, Cancer Research and Genetics UK (CRGUK), further securing the long-standing partnership which has seen the CRGUK donate over £70,000 to the University to help fund vital cancer research. Colorectal cancer is a major health issue worldwide, usually treated with surgery, radiotherapy, or drugs. Cardiff’s researchers are interested in how the body handles these drugs. In some other cancers, certain proteins, which are called ‘transporters,’ are really important for treatment. We do not know much about their role in colorectal cancer yet, but early studies suggest they could be key in determining how a patient responds to their treatment. The research could improve the way colorectal cancer is treated, offering patients more effective, personalised care and a better chance at a longer, healthier life.
Colorectal cancer is a major health issue worldwide, usually treated with surgery, radiotherapy, or drugs. Cardiff’s researchers are interested in how the body handles these drugs. In some other cancers, certain proteins, which are called ‘transporters,’ are really important for treatment. We do not know much about their role in colorectal cancer yet, but early studies suggest they could be key in determining how a patient responds to their treatment. The research could improve the way colorectal cancer is treated, offering patients more effective, personalised care and a better chance at a longer, healthier life.